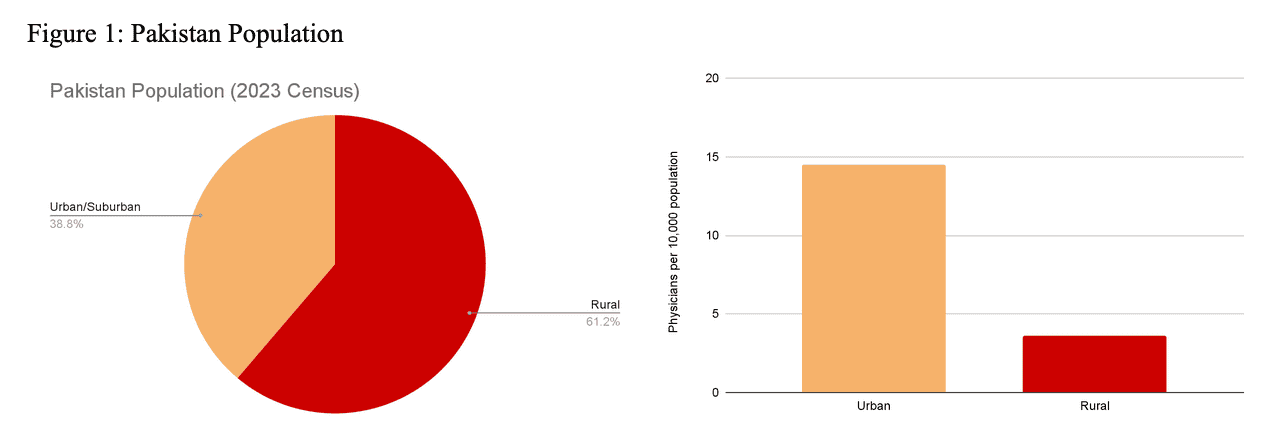
While 61% of Pakistan’s population lives in rural areas, per the 2023 Pakistan Census Report, there remains a deficiency in access to healthcare in these rural areas (Figure 1) 1. There are only 3.6 physicians per 10,000 people in rural areas when compared to 14.5 physicians per 10,000 people in urban areas 2. Challenges such as violence against healthcare workers, poor infrastructure, lack of employment opportunities, and inadequate facilities deter urban healthcare workers from practicing in rural areas 3. Many rural healthcare centers lack hygiene, infrastructure, and equipment. This results in limited access to care, especially for time-sensitive illnesses 3,4. This is compounded by a shortage of emergency medicine-trained physicians in Pakistan as there are only thirteen emergency medicine residency programs in the country 5.
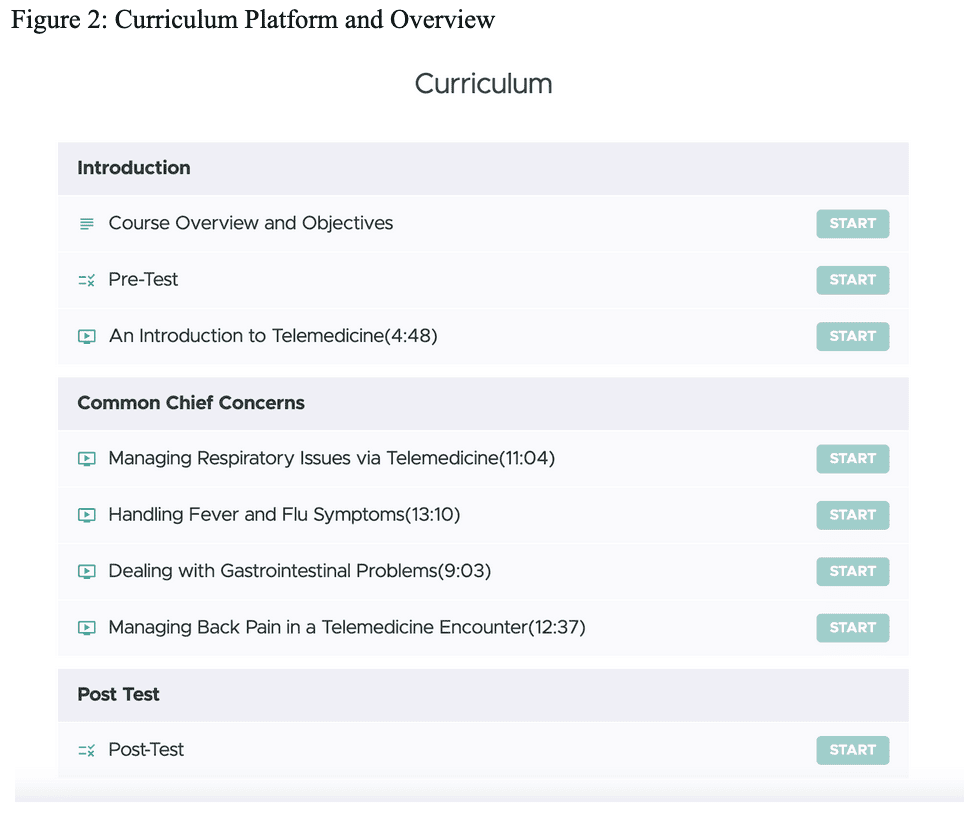
More recently, multiple asynchronous and synchronous telemedicine initiatives have been implemented in Pakistan, with several focusing on care for rural areas. However, there is no current initiative to close the gap between the need for emergency medical services and the lack of providers in rural areas. Our mission at Health Tech Without Borders (HTWB) is to close this gap by connecting urban providers to rural patients requiring urgent care. Given the lack of emergency medicine-trained providers, we created a telemedicine curriculum targeted to train Pakistan-based physicians of all backgrounds and specialties on practicing urgent care. Our telemedicine course consists of a twenty-question pre-test, an introduction to telemedicine primer video including how to set up for a telemedicine visit, and videos focused on four common chief complaints that are appropriate for telemedicine, including diarrhea, cough and respiratory tract infections, fever, and back pain. The course concludes with a twenty question post-test followed by a course survey (Figure 2). Course participants have to score 80% or higher on the post-test to pass the course and receive their certificate. Our course is located on the platform Teachable, and is free for all participants.
Our organization, Health Tech Without Borders, is a non-profit organization dedicated to expanding the reach of healthcare globally through innovative and digital means. We partnered with a local Pakistani telemedicine company, Oladoc, to distribute our course with their physician employees. Oladoc is providing HTWB with an encrypted telemedicine platform through which we can provide synchronous video and audio telemedicine. This company operates in all major cities in Pakistan. There are three parts to our project. The first step of our project is to distribute our course through Oladoc to physicians interested in learning more about/ practicing urgent care telemedicine. The second step of our project is to pilot encounters between physicians and patients in medium to large city settings. Once this phase is complete, we plan to expand our reach to connect urban providers with patients in rural settings.
Our goal is to provide a mode of healthcare for rural populations, focusing on those who do not currently have any access to care in their geographical regions. We hope to allow for a robust yet efficient and more standardized method of providing urgent care while promoting digital approaches to medicine in Pakistan.
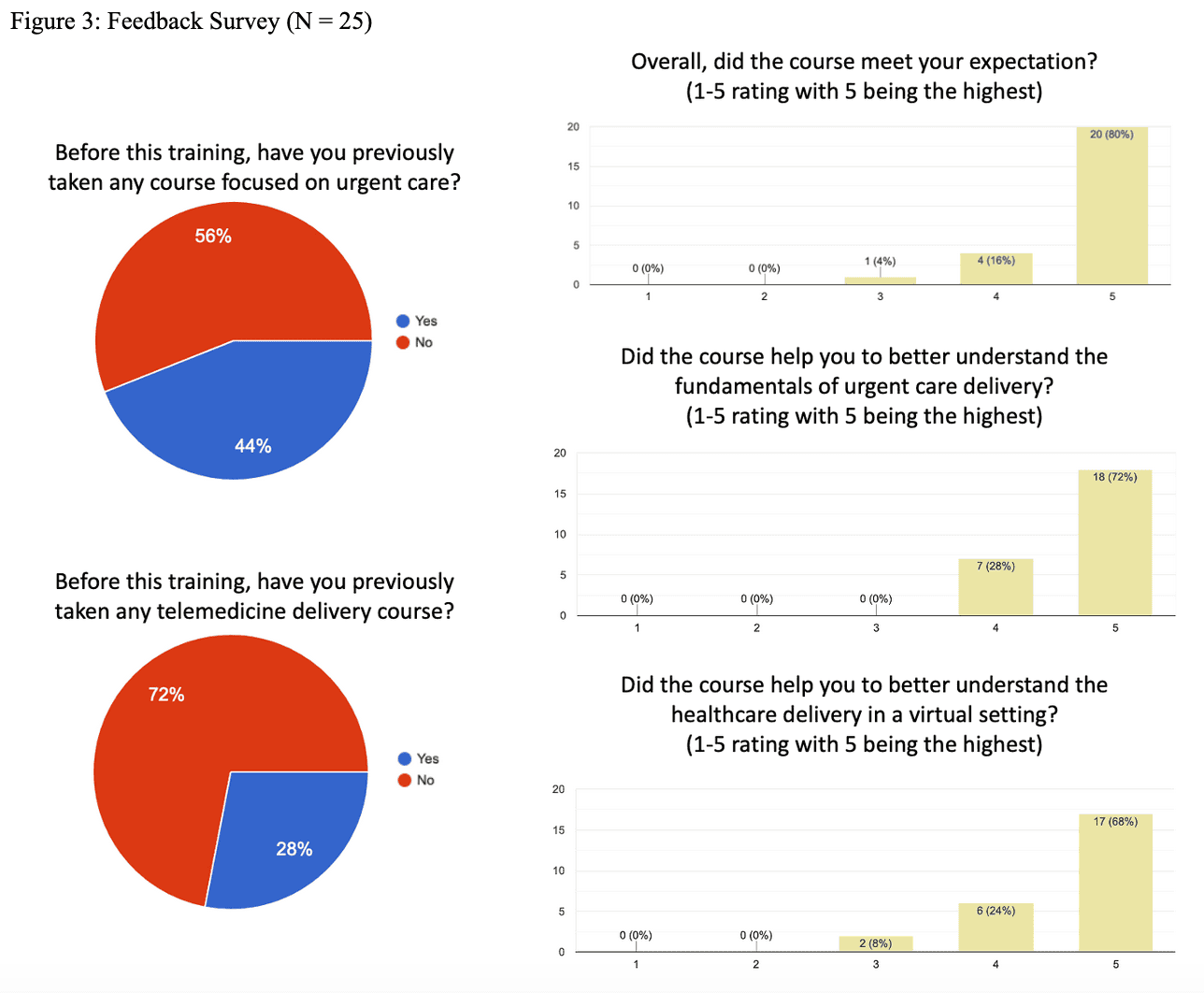
As of May 4, 2024, 157 physicians are actively enrolled in the curriculum. Initial findings indicate that while the majority are general practitioners, the participant pool has a diverse array of backgrounds. Remarkably, 72% of them have never received formal training in telemedicine. Feedback from the participants has been overwhelmingly positive: 96% reported that the course met their expectations, 92% acknowledged its role in enhancing their comprehension of virtual healthcare delivery, and all respondents agreed that it deepened their understanding of urgent care principles (Figure 3). Considering that most participants lack specialized training in urgent care, these findings are promising, suggesting the efficacy of standardized telemedicine education for future practitioners.
In conclusion, the current telemedicine initiatives mark just the beginning of our journey towards equitable healthcare access in rural Pakistan. Moving forward, we are committed to expanding our reach, refining our curriculum, and fostering partnerships to ensure timely and quality access to healthcare.
References
- ANNOUNCEMENT OF RESULTS OF 7TH POPULATION AND HOUSING CENSUS-2023 . (2023, August 5). https://www.pbs.gov.pk/sites/default/files/population/2023/Press%20Release.pdf
- Khalil, M., & Alameddine, M. (2020). Recruitment and retention strategies, policies, and their barriers: A narrative review in the Eastern Mediterranean Region. Health science reports, 3(4), e192. https://doi.org/10.1002/hsr2.192
- Jaffry, T. N., Mirza, S., Farheen, S., & Khalid, S. (2017). RELUCTANCE TO SERVE IN RURAL AREAS: DOCTORS’ PERSPECTIVE. Pakistan Journal of Public Health, 7(3), 157–162.
- Muhammad, Q., Eiman, H., Fazal, F., Ibrahim, M., & Gondal, M. F. (2023). Healthcare in Pakistan: Navigating Challenges and Building a Brighter Future. Cureus, 15(6), e40218. https://doi.org/10.7759/cureus.40218
- Saleem, S. G., Ali, S., Khatri, A., Mukhtar, S., Farooq, W., Maroof, Q., Jamal, M. I., Aziz, T., Haider, K. F., Dadabhoy, F. Z., & Rybarczyk, M. M. (2023). Clinical outcomes following the implementation of a novel one-year training program in emergency medicine in Karachi, Pakistan. Annals of Global Health, 89(1). https://doi.org/10.5334/aogh.3890


